ADHD Overview

Attention-Deficit Hyperactivity Disorder is a neurodevelopmental disorder that affects about 5-7% of adults. As an adult, ADHD is often revealed during major life events such as: Starting post-secondary Career advancement Changes to family dynamics (beginning or separating a family) Menopause Retirement These are a few of life events which may uncover your ADHD. It is important to note that ADHD is not an intellectual disorder; you can have ADHD, a high IQ and still be negatively impacted by ADHD. The underlying symptoms of ADHD are the same, however, the impairments present differently in everyday life from person to person. Adults with ADHD can experience academic failure, occupational difficulties, numerous job changes, relationship problems, financial difficulties, and substance use. In most adults, ADHD is often accompanied by a co-existing condition such as anxiety or depression. Some other ways ADHD might show up in a person’s life: Having difficulty with focus during conversations; my mind is elsewhere Feeling like you are not working to your potential or underachieving Working significantly harder than your peers to achieve the same results Feeling frustrated and impatient, having emotional outbursts Not being able to finish reading an article or book Being easily distracted by the sights and sounds in the environment Over or under estimating time required to complete tasks Hyper-focusing on a task while ignoring surroundings Procrastinating or delaying the start of important tasks Impulsive spending, eating, drinking, or sexual activity Frequent driving accidents or traffic tickets Poor organization Forgetful in daily activities Consistently loses or misplaces things such as keys, wallet or glasses ADHD is highly heritable and if one family member has ADHD, it is likely that another member also has ADHD. The exact cause of ADHD is still unknown; we do know that there are differences in the brains of people who have ADHD compared to those who do not. The ADHD Brain is different than the non-ADHD Brain A Pet Scan illustrating difference between a brain with ADHD and one without. PHOTO: NEUROSCIENCENEWS What is different in the ADHD brain? The ADHD brain structure is different:It is smaller, has less volume in some brain regions, and has less cortical thicknessThe ADHD brain functions differently:Less activation of networks needed for executive function and attention. Excessive activation of networks causing hyperactivity and impulsivity.The ADHD brain has problems with some pathways: The neurotransmitters dopamine and norepinephrine; brain pathways are not working well. The Adult ADHD Self-Report Scale (ASRS-v1.1) Symptom Checklist is a tool that healthcare providers may use to screen for Adult ADHD. This is not a diagnostic tool but a screener to indicate if a further detailed assessment is necessary. Although we do not use this screener at our Centre, you may download a free Adult ADHD Self-Report scale below. Download ASRS
Work And School Strategies

Strategies to Succeed at Work Adults with ADHD often self-select careers using the advantageous traits of their ADHD to succeed, however, often at least one of their ADHD traits will negatively impact an aspect of the job or with colleague/supervisor interpersonal relationships. It is important to be aware of the areas of ADHD that impact your work to develop better ways to support yourself for success.
Schedule and Routines

Schedules and Routines ADHD often involves difficulties with organization, time management, and maintaining focus. Structured schedules and routines can mitigate these challenges by providing a predictable framework within which to operate. Consider implementing routines for tasks such as:– Eating/meals,– Exercise,– Sleeping,– Appointments,– Medication– Social events.
Gadgets and Tools

Use Gadgets and Tools to Manage Your ADHD There are a lot of ADHD management tools that are marked for adults. It is important to select and trial supports that may help you. When selecting a gadget or tool, consider your challenge areas and look for something affordable and easy to use. Trial your selection and if it does not work, identify why and re-adjust by selecting another support that will be better suited. Some examples of tools and gadgets are:– To-Do lists/planners– Apps for phones and tablets– Spreadsheets– Whiteboards– Digital recorders– Calendar reminders for appointments– Program routines and schedules into cellular phones
Healthy Living

Exercise, Sleep and Meditation Exercise Not only is regular exercise good for physical health but it is helpful for mood, anxiety and focus Try to fit regular exercise into your weekly routine At work, stand more and sit less Implement exercise routines with a trainer or by attending an exercise class Use metrics to monitor your health and exercise success by: Measuring daily weight Counting steps or distance walked Using a watch to monitor heart rate, activity and sleep Sleep People with ADHD can have difficulty falling asleep and staying asleep Treatment of ADHD often leads to improved sleep Practice good sleep hygiene: Follow a consistent sleep schedule including going to sleep and waking up at the same time daily Ensure the bedroom is quiet, dark and with the correct room temperature Avoid overstimulation before sleep time, such as television, video games and online chatting Avoid caffeine products in the afternoon and evening Meditation, Yoga and Breathing Exercises Many people find that meditation, yoga, and breathing exercises help with focus and anxiety Meditation and yoga classes can be attended in studios but also be done at home with videos and apps Try to schedule these wellness breaks into your daily routine
Substance Use

ADHD and Substance Use Alcohol and cannabis can interfere with the effectiveness of ADHD stimulant medication.Coffee, tea, energy drinks and other caffeine products can lead to “overstimulation” if taken with ADHD stimulant medication. Remember to discuss the use of all recreational substances and over-the-counter medications with your physician/nurse practitioner
ADHD Medication

ADHD Medication First Line ADHD Treatments ADHD & ADD medication is an important part of ADHD management strategy along with the non-medicine strategies. ADHD medication has been around for more than fifty years and there are many published research papers on their safety and efficacy. First-line treatment guidelines for ADHD and ADD medication are stimulant medication either a Methylphenidate or Amphetamine product. There are many different options within these two categories. ADHD stimulants work by blocking the reuptake of norepinephrine and dopamine within the brain. While Amphetamine also promotes the release of norepinephrine and dopamine. Canadian Stimulant Options The medication, doses and possible side effects listed here are for educational purposes only. You should talk to your healthcare provider about the medication options available, their benefit and possible side effects. Medication should only be started/changed/adjusted by a patient’s physician or nurse practitioner. Methylphenidate (Ritalin) Based Amphetamine (Dexedrine) Based Possible Medication Side Effects Medication management is usually effective with minimal side effects, some side effects may go away in time. It is always important to discuss with your doctor the benefits and side effects when starting any medication. Palpitations Increased heart rate Irregular heart rhythm Increased blood pressure Sleep disturbance Decreased appetite Increased anxiety/ irritability Headache Dry mouth Chest pain Rashes ADHD Medications Usually Help to Please see CADDRA guide to ADHD pharmacological treatments in Canada – updated October 2024. Click here
How Life Stages Affect Women’s Focus

For women with ADHD, the hormonal changes that come with various life stages can significantly impact how symptoms present and how manageable they feel. From the menstrual cycle to pregnancy and postpartum, hormone fluctuations can lead to challenges in focus, mood regulation, and emotional balance. Understanding how these shifts affect ADHD can help women develop strategies to navigate these changes more effectively. The Menstrual Cycle and ADHD The menstrual cycle plays a key role in influencing ADHD symptoms. During the first two weeks of the cycle, rising estrogen levels are associated with improved mood, cognitive function, and focus. Many women with ADHD feel more in control and find it easier to manage their symptoms during this phase. However, the story changes after ovulation, when estrogen levels drop, and progesterone levels rise. This hormonal shift leads to a decline in dopamine, a neurotransmitter that plays a crucial role in attention and executive function. As a result, many women experience a worsening of ADHD symptoms in the premenstrual phase, including increased difficulty with focus, emotional regulation, and impulsivity. These changes can feel frustrating, as the ebb and flow of hormones can make it seem like symptoms vary drastically throughout the month. Puberty and ADHD Puberty brings another significant wave of hormonal change, particularly with the surge of estrogen and progesterone. For girls with ADHD, these changes can intensify symptoms. Emotional volatility, mood swings, and increased difficulty with attention and impulse control are common during this time. Puberty also coincides with social and academic pressures, which can make managing ADHD symptoms even more challenging. Parents and educators play a critical role during this period by offering understanding, support, and potentially adjusting treatment strategies. It’s important to recognize that ADHD management may need to evolve as a girl transitions through puberty, as the combination of hormonal changes and environmental demands can complicate symptom control. Pregnancy and ADHD Challenges Pregnancy presents unique challenges for women with ADHD. The dramatic hormonal changes that occur during pregnancy can affect mood and cognitive function, often leading to worsened ADHD symptoms. Many women also face the dilemma of whether to continue ADHD medications during pregnancy due to concerns about their safety. Balancing the benefits and risks of continuing medication can be difficult, and decisions should be made in close consultation with healthcare providers. For those who choose to pause medication, non-pharmacological strategies like cognitive-behavioral therapy (CBT) and lifestyle adjustments can be particularly helpful. It’s important to stay flexible and explore alternative treatments to manage symptoms during this time. The Postpartum Period and ADHD The postpartum period is an especially challenging time for women with ADHD. Hormonal fluctuations, combined with sleep deprivation and the demands of caring for a newborn, can significantly exacerbate symptoms. Focus, organization, and emotional regulation may become even more difficult, making the early months of motherhood overwhelming. Support from healthcare providers, family, and friends is crucial during this period. Establishing routines, seeking help with childcare, and leaning on a support network can all help mitigate some of the stress that comes with being a new mother while managing ADHD. Open communication with healthcare professionals about any changes in symptoms can also ensure that appropriate treatment plans are in place. Managing ADHD Across Life Stages No matter the life stage, managing ADHD effectively often requires a combination of medical treatment and lifestyle adjustments. Regular exercise, maintaining a balanced diet, and good sleep hygiene are essential components of overall brain health and can help reduce the impact of hormonal fluctuations. Cognitive-behavioral therapy (CBT) can be particularly helpful for women dealing with stress and emotional regulation challenges that arise from hormonal changes. This type of therapy provides strategies for managing negative thought patterns and improving organizational skills, making it easier to cope with the complexities of ADHD. Tracking symptom patterns in a diary can help women and their healthcare providers identify how hormonal shifts affect ADHD symptoms. Adjusting medication and treatment plans based on these patterns allows for more tailored management strategies, ensuring that symptoms remain under control even during hormonal transitions. The Role of Estrogen in ADHD Estrogen plays a significant role in regulating neurotransmitters like dopamine, serotonin, and norepinephrine, all of which are involved in attention, mood, and cognitive function. Higher levels of estrogen are often associated with improved attention and executive functioning, while lower levels can exacerbate ADHD symptoms. This understanding helps explain why many women experience relief from symptoms during certain phases of their menstrual cycle or during life stages when estrogen levels are higher. Conversely, periods of low estrogen, such as during the premenstrual phase or postpartum—can lead to more pronounced symptoms. Building a Strong Support System In addition to medical treatments and lifestyle changes, building a strong support system is crucial for women with ADHD. Support groups, whether in-person or online, can provide valuable insight and a sense of community. Women can share experiences, exchange strategies, and learn from others who are navigating similar challenges. Healthcare providers, including ADHD specialists and therapists, offer another essential layer of support. Regular consultations with these professionals ensure that treatment plans remain effective and can be adjusted as needed. Educational resources, such as books and reputable websites, also provide useful information on managing ADHD at different life stages. The impact of hormonal changes on ADHD symptoms is undeniable, but with the right strategies and support, women can navigate these fluctuations more effectively. By understanding how hormones influence ADHD symptoms, adjusting treatment plans, and building a strong support network, women can take control of their health and better manage ADHD across the different stages of life.
Untangling Menopause and ADHD

Menopause is a significant life transition that brings about a range of physical and emotional changes, and for women with ADHD, it can present unique challenges. As estrogen and progesterone levels decline, many women find that their ADHD symptoms intensify. Here’s a look at how menopause impacts ADHD, why diagnosing and treating the condition can be particularly challenging during this time, and effective strategies to manage symptoms. The Impact of Menopause on ADHD Symptoms Menopause triggers a substantial shift in hormone levels, notably a decrease in estrogen and progesterone. These hormones play an important role in regulating neurotransmitters like dopamine and serotonin, which are essential for managing attention, focus, and mood. As hormonal levels fluctuate and eventually decline, many women with ADHD may notice a worsening of symptoms such as difficulties with concentration, memory lapses, and challenges with emotional regulation. Additionally, the stress and sleep disturbances commonly associated with menopause can further exacerbate these symptoms. The Challenge of Diagnosing ADHD During Menopause Diagnosing ADHD during menopause can be complex due to the overlap in symptoms. Both menopause and ADHD can present with difficulty concentrating, irritability, and mood swings, making it challenging to differentiate between the two. For women who have never been previously diagnosed with ADHD, it can be particularly confusing to recognize these symptoms as related to ADHD rather than attributing them solely to menopause. The lack of awareness about ADHD in adult women adds another layer of difficulty to the diagnostic process. The Complexities of Treatment Treating ADHD during menopause involves navigating the interplay between hormonal changes and ADHD medication. Hormonal fluctuations can impact how women respond to ADHD treatments, with the effectiveness of stimulant medications potentially varying throughout different stages of menopause. Additionally, managing ADHD alongside menopausal symptoms often requires a multifaceted approach. This may include hormone replacement therapy (HRT), lifestyle adjustments, and careful monitoring of medication efficacy and side effects. Coordinating these treatments requires a nuanced approach to avoid adverse effects and ensure comprehensive care. How Common is the Worsening of ADHD Symptoms During Menopause? Research indicates that it is relatively common for women with ADHD to experience a worsening of symptoms during menopause. A survey found that 94% of women with ADHD reported increased difficulties during perimenopause and menopause. This suggests that hormonal fluctuations significantly impact ADHD symptoms, though the exact prevalence can vary. More research is needed to fully understand the extent of these effects. Strategies for Managing ADHD Symptoms During Menopause Effective management of ADHD symptoms during menopause involves a blend of medical and lifestyle strategies. Hormone replacement therapy (HRT) can help stabilize hormone levels, potentially alleviating some symptoms that overlap with ADHD, such as mood swings and cognitive difficulties. Additionally, maintaining a healthy lifestyle with regular exercise, a balanced diet, and good sleep hygiene supports overall brain health. Cognitive-behavioral therapy (CBT) and mindfulness practices are also valuable tools for managing both ADHD and menopausal symptoms. Regular consultations with healthcare providers are essential to adjust treatment plans as needed. Common Misconceptions About ADHD and Menopause Several misconceptions can hinder the understanding and treatment of ADHD in menopausal women. One common myth is that ADHD only affects children and is not relevant for adults, especially women. Another misconception is that menopausal symptoms are solely due to hormonal changes and not related to ADHD. These misunderstandings can lead to underdiagnosis and undertreatment. Additionally, the belief that ADHD symptoms improve with age is not always accurate, as symptoms may persist or even worsen. Advocating for Effective Treatment Women can advocate for their health by keeping detailed records of their symptoms and any changes they observe. Seeking out healthcare providers who are knowledgeable about both ADHD and menopause is crucial. Joining support groups and staying informed about the latest research can empower women to make informed decisions about their treatment. Being proactive in discussions with healthcare providers about all symptoms and treatment options is key to receiving effective care. Lifestyle Changes to Support ADHD Management Several lifestyle changes can be beneficial in managing ADHD symptoms during menopause. Regular exercise, a diet rich in omega-3 fatty acids, good sleep hygiene, and stress-reduction techniques such as yoga or meditation can all contribute to improved brain health. Staying organized with tools like planners and reminders can also help manage daily tasks more effectively. The Role of Hormone Replacement Therapy and Cognitive-Behavioral Therapy Hormone replacement therapy (HRT) can help stabilize hormone levels and reduce some of the menopausal symptoms that overlap with ADHD, such as mood swings and cognitive difficulties. However, it’s important to weigh the potential risks and benefits of HRT with a healthcare provider. Cognitive-behavioral therapy (CBT) is also a valuable tool for managing both ADHD and menopausal symptoms. CBT can help develop coping strategies, improve organizational skills, and address negative thought patterns, aiding in emotional regulation and daily functioning. Managing ADHD during menopause requires a comprehensive approach that addresses both hormonal changes and ADHD symptoms. By understanding the impact of menopause on ADHD and utilizing effective strategies, women can navigate this challenging period with greater ease and improve their overall quality of life.
Navigating the Intersection: ADHD and Menopause
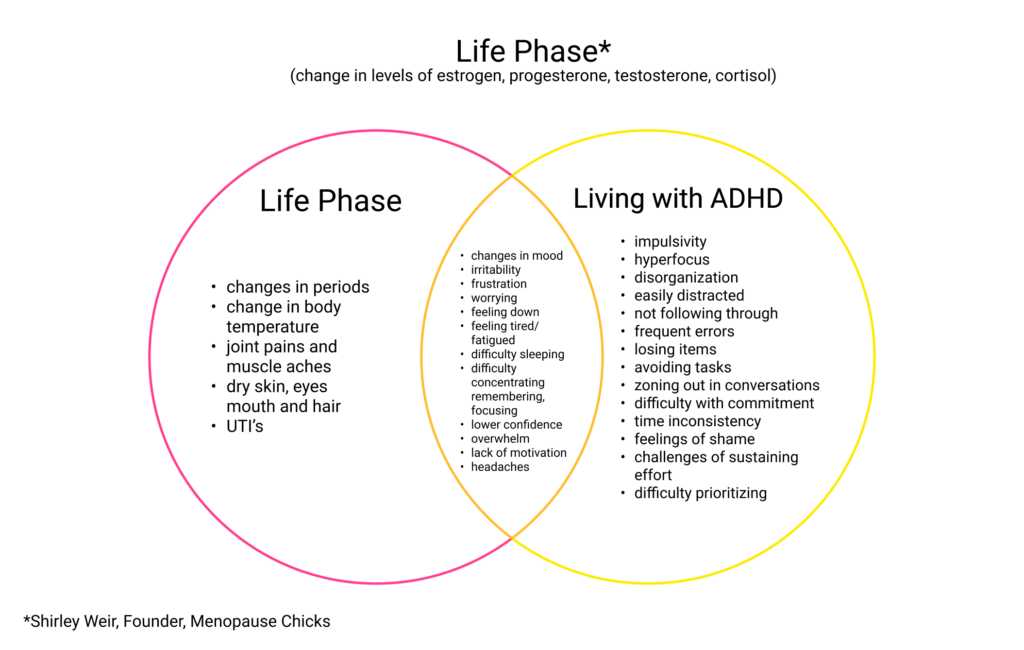
Both ADHD and menopause can profoundly affect women’s lives, often in overlapping ways that can make it difficult to distinguish between the two. While ADHD is a neurodevelopmental condition with symptoms like inattention, impulsivity, and executive dysfunction, menopause brings hormonal shifts that impact mood, memory, and cognitive function. These changes can exacerbate ADHD symptoms or even mimic them, leading to a unique set of challenges for women experiencing both. This diagram highlights the distinct symptoms of ADHD and menopause, while also illustrating the significant areas of overlap, offering insight into the shared struggles many women face.